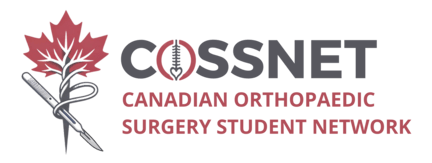
The Ottawa Ankle Rules are a set of guidelines developed to assist clinicians in deciding whether radiographic evaluation is necessary to rule out fractures in patients presenting with acute ankle and midfoot injuries. The primary purpose of these rules is to reduce the number of unnecessary radiographs, thus minimizing radiation exposure to patients and alleviating healthcare costs without missing clinically significant fractures.
The Ottawa Ankle Rules focus on the presence of pain in specific areas and the ability to bear weight both immediately after the injury and in the emergency department. According to the rules, an ankle radiograph series is only required if there is any pain in the malleolar zone and any one of the following criteria is met: bone tenderness at the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus, bone tenderness at the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus, or an inability to bear weight immediately after the injury and for four steps in the emergency department.
Similarly, a foot radiograph series is indicated if there is pain in the midfoot zone and any one of the following criteria is met: bone tenderness at the base of the fifth metatarsal, bone tenderness at the navicular bone, or an inability to bear weight immediately and in the ED for four steps.
These criteria have been validated through extensive research and have demonstrated high sensitivity for detecting fractures, making the Ottawa Ankle Rules a valuable tool in the clinical assessment of ankle and midfoot injuries. These rules are summarized in the above image from MDCalc, an excellent point-of-care reference.