Mason beaulieu, M3
University of saskatchwan
June 8th, 2025
Reviewed by Dr. Dawn Curran, R2
Memorial university
Radial Head & Ulnar Avulsion Fracture in a Male Hockey Player
Synopsis
A 28-year-old male presents to the emergency department after sustaining an isolated left upper extremity injury while playing ice hockey.
Plain radiographs revealed an oblique fracture of the radial head and an avulsion fracture of the proximal olecranon on CT.
The patient was treated with ORIF and recovered uneventfully.

Figure 1: a plain AP of the left elbow.

Figure 2: a plain oblique AP (in external rotation)

Figure 3: a 3D reconstruction CT.

Figure 4: Intra-op AP fluoroscopy.

Figure 5: Intra-op lateral fluoroscopy.
ID: "B" a 28-year-old male with a traumatic non-dominant left embow injury; otherwise healthy, non-smoker.
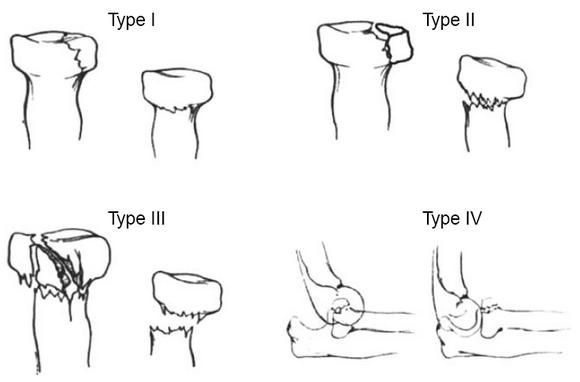
CC: Left radial head and ulnar fracture (Mason's Type II or III)
HPI: "B" was playing ice hockey when he skated full speed into the boards with his arms in 90° of flexion to brace himself for impact. There was no loss of consciousness. He immediately noticed a sharp, non-radiating pain to both forearms and wrists; however, the pain was more severe on his left, non-dominant side. He found he was unable to grip or manipulate his hockey stick. At this point, "B" skated back to the bench to watch the remainder of the game. He denied any pain to left shoulder or injury elsewhere. He did complain of some numbness to the dorsum of his left wrist and forearm which then subsided.
After the game, "B" presented to a walk-in clinic where the practitioner confirmed an isolated, left forearm fracture on plain radiographs. "B" was then provided a broad arm sling and encouraged to visit the emergency department to be seen by the orthopaedic team on call.
PMHx: Unremarkable.
Meds/allergies: The patient does not take any medications and has no known drug allergies.
PSHx: The patient has never had surgery.
Social Hx: "B" is a non-smoker and drinks alcohol occasionally. He denies any recreational drug use. He lives with his wife and young child. He works a desk job in sales.
P/E: On assessment, the patient appeared comfortable with a broad arm sling to his left upper extremity in situ. He was alert and oriented. All vital signs were stable. On exam, this was a closed injury with no obvious deformity. The left wrist and forearm were swollen and erythematous. The patient was tender to palpation over the dorsum of his left wrist and lateral aspect of his forearm. Elbow flexion and extension were limited secondary to pain, as was pronation/supination. He was neurovascularly intact to his left upper extremities (PIN, AIN, ulnar, axillary, musculocutaneous). Radial and ulnar pulses were strong and equal bilaterally. Cap refill was < 2 seconds and both hands were warm and well perfused. Dermatomal/myotomal functions were intact.
Imaging:
Figure 1: a plain AP of the left elbow.
Figure 2: a plain oblique AP in external rotation.
Figure 3: a 3D reconstruction CT.
These views were properly oriented and position. The films show an oblique fracture of the lateral aspect of the head of the radius that is slightly depressed resulting in a step deformity in the articular surface.
The 3D reconstruction CT shows a minimally displaced and comminuted but predominantly obliquely oriented intra-articular radial head fracture with a 2mm step deformity of the articular surface. There is also a displaced avulsion fracture of the supinator crest of the proximal olecranon with intra-articular extension to the radioulnar joint.
I/P: The case was reviewed with the staff orthopaedic trauma surgeon on call and the patient was consented for open reduction and internal fixation of the left proximal radius and ulna +/- a ligamentous repair of the left elbow.
The treatment plan was decided based on a Mason's type II or II classification radial head fracture which benefits from ORIF, particularly in young active patients such as "B".
Consent was received from the patient in the emergency department with the standard protocol of explaining the indications and potential benefits and risks of surgery including infection, bleeding, neurovascular injury, failure of hardware, non-union/malunion, and elbow stiffness, as well as treatment alternatives. All of "B's" questions were answered satisfactorily and he was then immobilized in a three-sided split with a cuff and collar for comfort. The patient received analgesic for breakthrough pain until day surgery.
The patient underwent ORIF one-week post injury. 2g of Ancef were given preoperatively for antibiotic prophylaxis. The fracture was confirmed intraoperatively. Anatomic reconstruction of the radial head was achieved using Acutrack 2 micro screws. The ulna was stabilized using an AO Synthes 4-hole mini modular locking LCDC plate which was then fixated using 2.0mm self-tapping cortical screws. The lateral ulnar collateral ligament was repairing with #2 Ultrabraid sutures. Figures 4 & 5 are intra-op AP and lateral fluoroscopy images which demonstrate acceptable anatomic reduction and fixation of the fractures. Examination intra-operatively demonstrated appropriate fixation of the lateral ulnar collateral ligament under stress testing. A full range of motion was achieved without instability with firm endpoints noted throughout elbow movement. The patient was transferred to recovery in stable condition and 2-week follow-up was unremarkable.