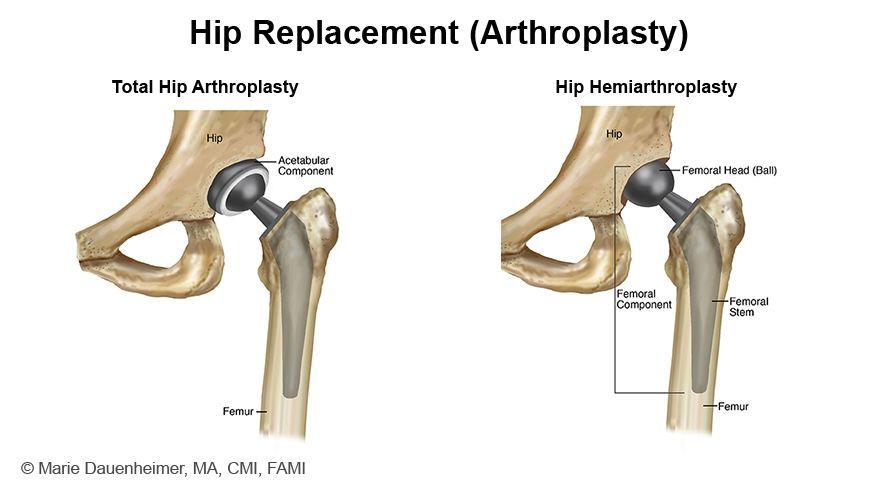
What is the difference between a total hip arthroplasty (THA) and hemiarthroplasty?
Total hip arthroplasty (THA) and hemiarthroplasty are both surgical procedures used to treat hip fractures, but they differ significantly in their approach, extent of replacement, and indications.
As you may recall, the hip is a “ball-and-socket” joint. THA involves the replacement of both the acetabulum (the hip socket) and the femoral head/neck (the ball). This procedure uses prosthetic components to replace the damaged parts of the hip joint, aiming to restore the function of the hip and relieve pain. THA is typically indicated for patients with hip fractures that are accompanied by pre-existing conditions such as osteoarthritis, rheumatoid arthritis, or any other degenerative changes in the hip joint that affect the acetabulum. It is also appropriate for younger, more active patients or those in whom longer-lasting joint durability is desired. The goal is not only to treat the fracture but also to address the underlying joint disease to improve overall joint function and longevity.
On the other hand, hemiarthroplasty involves the replacement of only the femoral head, while the acetabulum is left intact. This procedure is less extensive than THA and focuses on replacing the part of the hip joint that is directly affected by the fracture. Hemiarthroplasty is generally indicated for elderly patients with femoral neck fractures who do not have significant pre-existing arthritis or degenerative changes in the acetabulum. It is also suited for less active patients or those with a higher surgical risk, where the primary goal is pain relief and the restoration of mobility to allow for ambulation, rather than long-term durability of the joint.
In summary, the choice between THA and hemiarthroplasty for hip fractures is highly individualized, depending on the patient's clinical profile, underlying hip pathology, and functional demands. The ultimate goal is to provide the best possible outcome in terms of pain relief, mobility restoration, and joint function, tailored to the patient's specific needs and circumstances.
We covered the lateral approach to the hip in the episode, but can you describe the basics of the posterior approach to the hip?
The posterior approach is one of the most widely used methods for accessing the hip joint. It is relatively easy, safe, provides quick access to the joint, and can be performed with only one assistant. The approach is versatile and can be used for both hemiarthroplasty and total hip arthroplasty. The posterior approach also preserves the abductor mechanism, preventing loss of power post-operatively, and offers superior visualization of the femoral shaft, making it ideal for arthroplasty procedures where the femoral component needs to be replaced. However, it does involve division of the posterior capsule, increasing the risk of prosthesis dislocation through flexion and internal rotation.
Positioning:
Position the patient in a true lateral position with the surgical limb uppermost. Protect bony prominences with pads under the lateral malleolus and knee of the lower leg, as well as a pillow between the knees.
Landmarks and incision:
Identify the greater trochanter on the thigh's outer aspect, with its posterior edge being more superficial and palpable. Make a 10-15 cm curved incision centered on the posterior aspect of the greater trochanter, starting 6-8 cm above and posterior to it. Align the incision with the gluteus maximus fibers, curving it across the buttock and down the femoral shaft.
Superficial dissection:
The fascia lata on the lateral aspect of the femur is first incised to expose the vastus lateralis muscle. The fascial incision is then extended superiorly, aligning it with the initial skin incision. Following this, the gluteus maximus muscle fibers are split using blunt dissection. The gluteus maximus receives its blood supply from the superior and inferior gluteal arteries, so both arterial and venous bleeding should be anticipated. If the muscle is gently split, it allows for the crossing vessels to be picked up, coagulated, and cut before they are stretched and avulsed by the blunt dissection.
Deep dissection:
The split gluteus maximus fibers and deep fascia are retracted to expose the posterolateral hip joint, covered by short external rotator muscles attached to posterolateral proximal femur. The sciatic nerve runs down the back of the thigh over these muscles, encased in fat. The nerve crosses the obturator internus, the two gemelli, and the quadratus femoris before disappearing beneath the femoral attachment of the gluteus maximus.
To enhance visibility and protect the sciatic nerve, the hip is internally rotated, stretching the short external rotators. Stay sutures are placed in the piriformis and obturator internus tendons near the greater trochanter, and these muscles are detached slightly from their insertion and reflected back over the nerve. The quadratus femoris is usually left intact to avoid disturbing vessels from the medial circumflex artery. The capsulotomy is then performed with a longitudinal or T-shaped incision on the posterior capsule, allowing the hip to be dislocated with internal rotation, revealing the femoral head and neck.
Structures at risk:
In the posterior approach to hip surgery, the sciatic nerve and the inferior gluteal artery are structures at significant risk. The sciatic nerve, while not usually exposed, can be damaged by the compressive forces of retractors used to split the gluteus maximus. Occasionally, the sciatic nerve may split into tibial and common peroneal branches within the pelvis, necessitating careful identification to avoid missing a branch, which could lead to nerve damage. The inferior gluteal artery, exiting the pelvis beneath the piriformis and supplying the gluteus maximus, is also prone to injury. Its branches should be identified and coagulated to prevent bleeding.
Additional resources:
For an excellent training video from HSS detailing the posterior approach for total hip arthroplasty, performed on a cadaveric specimen, click
here.
For an outline of the posterior approach to the hip by AO Surgery Reference, click here.
For an outline of the direct lateral approach to the hip by AO Surgery Reference, as described in the podcast episode, click here.
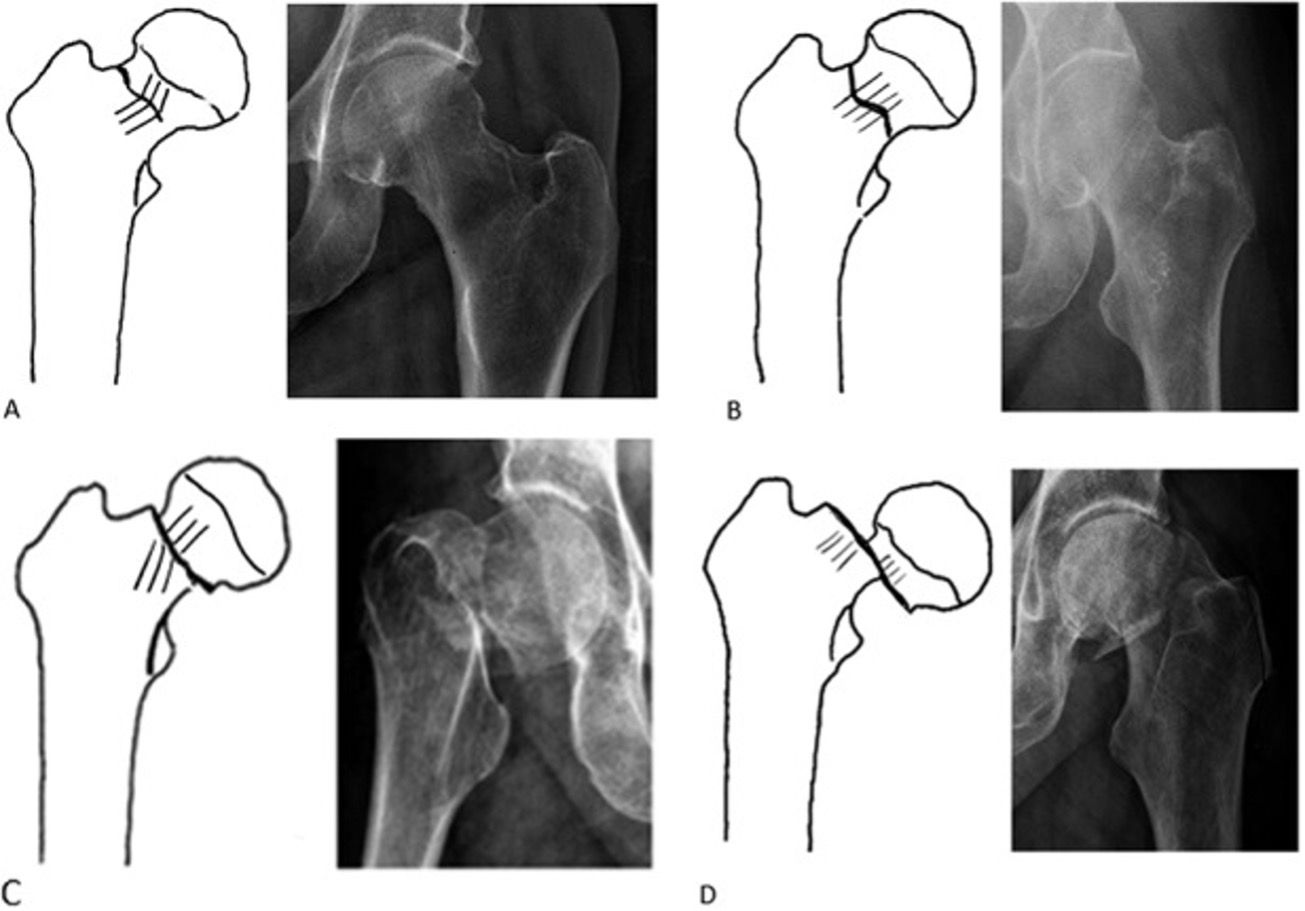
For intertrochanteric fractures, what are the indications for using a DHS vs. IMN?
As noted in our hip fracture decision tree, the management of intertrochanteric fractures may include an intramedullary nail (IMN) or a dynamic hip screw (DHS). This decision is guided by several anatomical and biomechanical considerations. These considerations influence the stability of the fracture fixation, the ability to bear weight, and the overall healing process. Below, we explore the reasons why the presence of an incompetent lateral wall, subtrochanteric extension, posteromedial comminution, and reverse obliquity would favor the use of an IMN over a DHS.