Advancements in Total Joint Replacement: Exploring Innovations in Orthopaedic Surgery
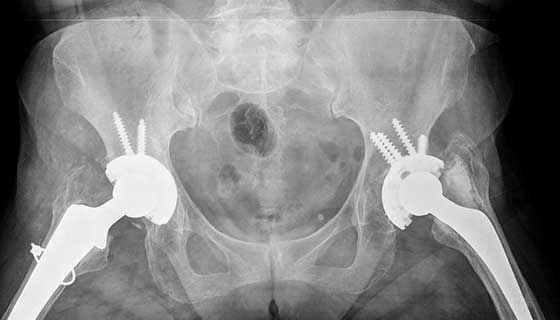
Orthopaedic surgery has witnessed remarkable advancements in recent years, particularly in the field of total joint replacement. As the aging population grows and demands for improved quality of life increase, orthopaedic surgeons are continually striving to enhance surgical techniques, implant designs, and post-operative care to optimize patient outcomes. In this blog post, we'll delve into some of the exciting innovations shaping the landscape of total joint replacement.
- Patient-Specific Implants: One size does not fit all when it comes to joint replacement. Patient-specific implants, custom-designed based on pre-operative imaging and anatomical measurements, offer a tailored solution for each individual. These implants improve fit, alignment, and longevity, ultimately leading to better functional outcomes and reduced complications.
- Robotic-Assisted Surgery: Robotics has revolutionized orthopaedic surgery by providing surgeons with enhanced precision and accuracy during total joint replacement procedures. Robotic-assisted systems allow for meticulous pre-operative planning, real-time intraoperative feedback, and optimal implant positioning, resulting in improved implant longevity and patient satisfaction.
- Advanced Implant Materials: The development of advanced implant materials, such as highly cross-linked polyethylene, ceramic-on-ceramic bearings, and oxidized zirconium, has significantly reduced wear rates and implant-related complications. These materials offer superior biocompatibility, reduced inflammatory response, and increased durability, leading to improved implant longevity and function.
- Minimally Invasive Techniques: Minimally invasive total joint replacement techniques have gained popularity due to their smaller incisions, reduced tissue trauma, and quicker recovery times. These techniques utilize specialized instruments and surgical approaches to minimize disruption to surrounding soft tissues while achieving optimal implant positioning and stability.
- Navigation Systems: Navigation systems provide real-time feedback to surgeons during total joint replacement procedures, enabling precise implant placement and alignment. By utilizing computer-assisted navigation, surgeons can achieve optimal biomechanics, reduce the risk of malalignment, and improve implant longevity, ultimately enhancing patient outcomes.
- Biological Augmentation: Biological augmentation techniques, such as platelet-rich plasma (PRP) therapy and mesenchymal stem cell (MSC) therapy, hold promise for enhancing tissue healing and promoting osteogenesis in total joint replacement patients. These biologic agents stimulate tissue regeneration, reduce inflammation, and accelerate the recovery process, leading to improved functional outcomes and faster return to activity.
- Patient-Centered Care Models: In addition to technological innovations, there has been a shift towards patient-centered care models in total joint replacement. Comprehensive pre-operative education, personalized rehabilitation protocols, and multidisciplinary care teams ensure that patients are actively engaged in their treatment plan and experience a seamless continuum of care from pre-operative preparation to post-operative recovery.
Advancements in total joint replacement have transformed the field of orthopaedic surgery, offering patients improved outcomes, enhanced longevity, and greater satisfaction. From patient-specific implants to robotic-assisted surgery and biologic augmentation techniques, orthopaedic surgeons have an array of innovative tools at their disposal to optimize surgical outcomes and improve quality of life for patients undergoing total joint replacement. As technology continues to evolve and research progresses, the future of orthopaedic surgery looks brighter than ever, promising further advancements and innovations to benefit patients worldwide.